Cancer Ablation by Water Vapor
The Vanquish® device’s thermal water vapor energy technology is a breakthrough therapy designed to use phase shift energy stored in sterile water vapor to convectively transfer thermal energy to cancerous tissue, causing cell death. Through this process, damage to surrounding structures is minimized or eliminated by respecting the prostate’s natural boundaries.
Vanquish aims to be a revolutionary cancer therapy that is tough on cancer yet gentle on patients.*
Phase Shift Energy in Water Vapor Technology
Cancer ablation by water vapor utilizes the vast amount of energy generated when liquid water changes to water vapor (steam).
As water converts to vapor or steam at ~100°C an exponential phase shift occurs, with the resulting water vapor carrying more than 5x the energy of water of the same mass.
During the ablation procedure, sterile water is converted to vapor and delivered through a needle-shaped catheter with a porous distal tip placed within the targeted tissue. Interstitial fluid-filled spaces surround prostate cells. In 10-second treatments, vapor exits the catheter at a higher pressure than the extracellular environment, moving convectively through prostatic tissue, displacing interstitial fluid, and reaching cell membranes. Rapid phase transformation of water vapor back to its liquid state (condensation) releases the stored latent heat of vaporization directly onto the affected cell membranes, denaturing them and causing cell death.

Vapor exiting the device
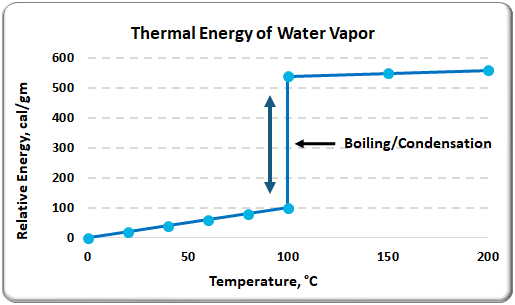
Water Thermal Energy = 1 cal/gm/°C
Vapor Thermal Energy = 539 cal/gm @100°C
Water Vapor Technology
Convection vs. Conduction:
Most of today’s ablative technologies utilize thermal energy emanating from a single point that is either hot or cold. The thermal energy then transfers from cell to cell (conduction) and gradually gets cooler (or warmer) the further you get from the source. This results in heating (or cooling) that is uneven and can be difficult to control.
Water vapor technology behaves very differently. When administered under pressure, the vapor moves through the interstitial space between the cells (convection) in a few seconds. The energy is evenly distributed throughout the vaporized area and ablates uniformly as the vapor condenses back into water.
Unlike conductive energy methods, vapor conforms to the prostate’s anatomy, optimizing thermal dose delivery to the targeted tissue and potentially minimizing damage to nerve bundles and surrounding structures. Convective heat transfer uniformly delivers thermal energy throughout the treatment region, unlike conductive ablation modalities that create thermal gradients.
Videos representing the difference between the conductive and convective transfers of thermal energy:
Respecting Natural Boundaries
The prostate, a walnut-sized gland located between the bladder and the penis just in front of the rectum, is encased within fibromuscular layers of cells called the prostate capsule. Within the prostate are areas (zones) separated by what are commonly referred to as pseudocapsules.
Traditional prostate cancer therapies can result in erectile dysfunction or urinary incontinence by damaging nerves or other tissue outside the prostate.1 In contrast, water vapor technology is uniquely designed to work inside the walls of the prostate, with the intent of minimizing or eliminating thermal damage to the nerves and surrounding prostate tissue.
A distinction between thermal water vapor and other ablative technologies: when vapor is released within one of the prostate zones, it intends to “respect” the boundaries of the prostate capsule and pseudocapsule by staying within the zone it was released into.
The ability to stay within the zone of application is critical when ablating prostate cancer because it will prevent the vapor’s ablative energy from escaping outside of the prostate.
By staying inside the targeted zone, the outcome should be a reduction in the incidences of erectile dysfunction and urinary incontinence commonly experienced with traditional prostate cancer therapies.
1] Prostate Cancer – Early-Stage: Symptoms, Diagnosis & Treatment – Urology Care Foundation. urologyhealth.org. Accessed June 15, 2024. https://urologyhealth.org/urology-a-z/p/prostate-cancer.
Respecting Natural Boundaries
The prostate, a walnut-sized gland located between the bladder and the penis just in front of the rectum, is encased within fibromuscular layers of cells called the prostate capsule. Within the prostate are areas (zones) separated by what are commonly referred to as pseudocapsules.
Traditional prostate cancer therapies can result in erectile dysfunction or urinary incontinence by damaging nerves or other tissue outside the prostate.1 In contrast, water vapor technology is uniquely designed to work inside the walls of the prostate, with the intent of minimizing or eliminating thermal damage to the nerves and surrounding prostate tissue.
A distinction between thermal water vapor and other ablative technologies: when vapor is released within one of the prostate zones, it intends to “respect” the boundaries of the prostate capsule and pseudocapsule by staying within the zone it was released into.
The ability to stay within the zone of application is critical when ablating prostate cancer because it will prevent the vapor’s ablative energy from escaping outside of the prostate.
By staying inside the targeted zone, the outcome should be a reduction in the incidences of erectile dysfunction and urinary incontinence commonly experienced with traditional prostate cancer therapies.
1] Prostate Cancer – Early-Stage: Symptoms, Diagnosis & Treatment – Urology Care Foundation. urologyhealth.org. Accessed June 15, 2024. https://urologyhealth.org/urology-a-z/p/prostate-cancer.
*CAUTION Investigational device. Limited by United States law to investigational use.
Improving Quality of Life
“The vision that started this company and continues to drive us is to create a better experience for the patient. Water vapor is an ideal tool for accomplishing this goal. It is simple, natural, and gentle, but powerful.”

